Tour (1 of 7)
Food Sensitivities: An Under-Diagnosed Source of Inflammation & Symptoms
W.T. Knicker, MD Past Chairperson Adverse Food Reactions Committee American College of Allergy, Asthma & Immunology

- Irritable bowel
- Migraine
- Fibromyalgia
- Attention deficit
- Hyperactivity
- Obesity
- And many other challenging conditions
Fully addressing sensitivities can produce a major improvement in outcomes, especially in your treatment resistant patients.
Tour (2 of 7)
A Recent Breakthrough in Understanding
Dr. Mark J. Pasula Past Chairperson Adverse Food Reactions Committee American College of Allergy, Asthma & Immunology
Recent research proves that sensitivities often involve the innate immune system, a branch of the immune system which has been totally overlooked the past 40 years as a category of adverse food reactions.
An important 2011 study comparing 2 different types of gluten reactions– celiac disease and gluten sensitivity was the first study to confirm the role of the innate immune system in gluten reactivity.

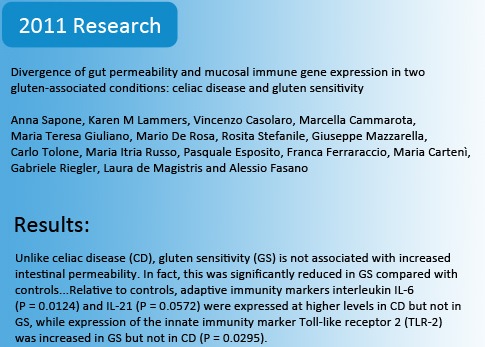
- It showed that gluten sensitivity is a distinct clinical entity entirely different than celiac disease or wheat allergy.
- Where celiac disease affects 1 in 133, gluten sensitivity is 6-8 times more prevalent, affecting an estimated 15-20 million Americans
- Where the inflammatory process in celiac disease is governed by the adaptive immune system, it showed that the innate immune system governs reactions in gluten sensitivity, a fact previously unknown. This understanding is critical because for decades, all allergy research has completely neglected the role of the innate immune system in food-induced inflammation.
- It showed that the commonly held belief that food sensitivities are the result of a “leaky gut” was not entirely correct. In fact, this study showed less gut permeability in the gluten sensitive patients than in the controls. This means that in order for food sensitivities to manifest, increased gut permeability doesn’t have to be involved and may not be at all. However, if leaky gut is involved, then the development of food sensitivities is practically certain.
Reactivity to gluten is just one potential part of the inflammatory puzzle. We know through our experience with tens of thousands of food sensitive patients that even so called “anti-inflammatory” foods, such as salmon, blueberries, parsley, garlic, lettuce, even turmeric and ginger, and virtually every other “healthy” food can trigger inflammatory reactions that contribute to illness. Optimizing outcomes is only possible if you have the full picture of each patient’s individual sensitivities.
Tour (3 of 7)
Food-Chemical Reactions Are Clinically Significant
 Inflammatory reactions to naturally occurring or artificial food-chemicals are another area of consideration. Conditions like migraine, ADD/ADHD, and others, in addition to food sensitivities, often have clinically significant reactions to food-chemicals. These reactions are not antibody mediated and thus cannot be identified with IgG, IgA or IgE testing.
Inflammatory reactions to naturally occurring or artificial food-chemicals are another area of consideration. Conditions like migraine, ADD/ADHD, and others, in addition to food sensitivities, often have clinically significant reactions to food-chemicals. These reactions are not antibody mediated and thus cannot be identified with IgG, IgA or IgE testing.
These inflammation-provoking and symptom-provoking reactions are as clinically relevant as reactions to gluten, and continued consumption of offending foods and food-chemicals is a major obstacle in achieving optimal outcomes.
Certain foods and beverages, such as aged cheese, alcoholic beverages, and food additives such as nitrates (in pepperoni, hot dogs, luncheon meats) and monosodium glutamate (MSG, commonly found in Chinese food) may be responsible for triggering up to 30% of migraines.¹
Tour (4 of 7)
The Patented MRT®: The Most Effective Way to Identify Hidden Inflammatory Foods
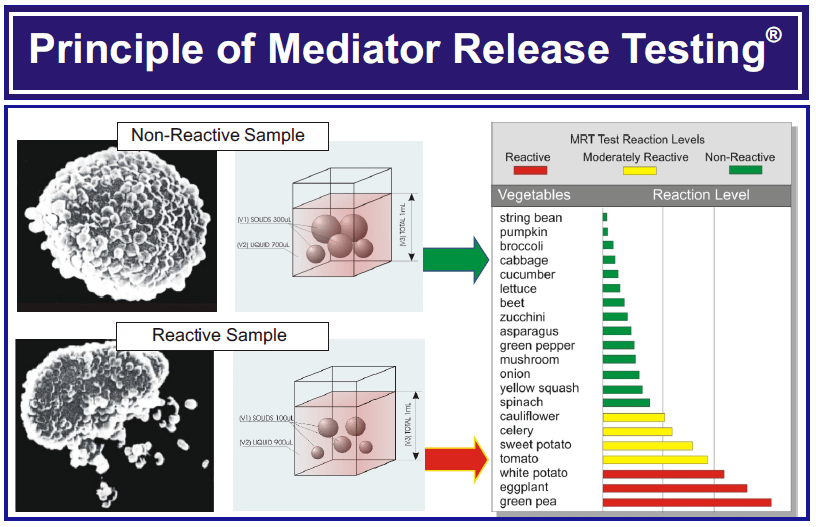
Despite all the immunologic and clinical complexities associated with food sensitivities, the scientific fact is that white blood cells are always involved in food-induced inflammatory reactions. It’s the cytokines, prostaglandins, leukotrienes and other mediators released from various white cells that cause every negative effect your patients suffer. This is true whether reactions involve the adaptive or innate immune system, whether reactions are cell-mediated or humorally mediated, whether symptoms are immediate or delayed, whether reactions are dose-dependent or not, and whether potential mechanisms are elevated or not.
Through Oxford, the patented Mediator Release Test (MRT®) delivers unparalleled information that no other blood test or approach provides. MRT® is a functional assessment of the inflammatory response that takes into consideration the widest range of sensitivity mechanisms. And because MRT® quantifies the inflammatory response, it is able to shed light on both clinical and sub-clinical inflammatory reactions.
MRT® is the most reliable and clinically useful food sensitivity test that exists and forms the basis for the LEAP Anti-Inflammatory Eating Plan. Subclinical reactions often relate to the dose dependent nature of food and food-chemical reactions. When designing an anti-inflammatory eating plan for your patient that will produce the most complete outcomes in the shortest time, you need to know both. This critical information can only be provided by MRT®.
Tour (5 of 7)
LEAP Anti-Inflammatory Eating Plan
- LEAP maximizes the value of the information MRT® provides
- Incorporates the patient’s history
- Includes the patient’s food preferences
- Is easier to follow
- And gets greater patient buy-in and adherence and consistently produces the best outcomes in the shortest time

Tour (6 of 7)
LEAP: The Most Complete Outcomes in the Shortest Time
 The MRT®-based LEAP anti-inflammatory eating plan routinely produces the most complete outcomes in the shortest time. Common food sensitivity related conditions typically achieve rapid, lasting relief in as little as 5-7 days. In fact, in properly selected patients, it is highly uncommon to not see a noticeable change in just 2 weeks.
The MRT®-based LEAP anti-inflammatory eating plan routinely produces the most complete outcomes in the shortest time. Common food sensitivity related conditions typically achieve rapid, lasting relief in as little as 5-7 days. In fact, in properly selected patients, it is highly uncommon to not see a noticeable change in just 2 weeks.
The benefits of LEAP and MRT® go far beyond food sensitivity related health problems; it empowers the patient to take an active part in their care, and it helps the patients realize a sense of control over their health that they otherwise wouldn’t have. They no longer feel a victim to things beyond their control.
If you’re a practitioner that wants the consistently best outcomes, the best food sensitivity blood test, and the easiest and most effective eating plan, then click here to have an Oxford Representative contact you to setup MRT® and LEAP in your practice.
